Журнал «Медицина неотложных состояний» Том 20, №5, 2024
Вернуться к номеру
Як запобігти ускладненням при лапароскопічній холецистектомії: критичний погляд на безпеку
Авторы: Чуклін С.М., Чуклін С.С.
Медичний центр Святої Параскеви, м. Львів, Україна
Рубрики: Медицина неотложных состояний
Разделы: Справочник специалиста
Версия для печати
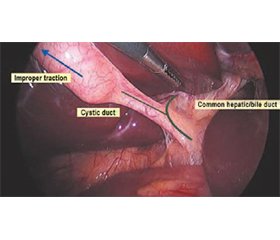
Лапароскопічна холецистектомія пов’язана з вищою частотою ушкоджень жовчних шляхів і судин, ніж відкрита холецистектомія. Анатомічне неправильне сприйняття є найпоширенішим основним механізмом таких травм. Доведено, що критичний погляд на безпеку (CVS) є хорошим способом отримання надійної анатомічної ідентифікації. Його настійно пропонують різні рекомендації. Концептуально CVS — це метод ідентифікації мішеней, причому мішенями є дві міхурові структури. Це передбачає три основні кроки, а саме: 1) повне очищення печінково-міхурового трикутника від фіброзно-жирової тканини, 2) відокремлення нижньої частини жовчного міхура від міхурової пластинки так, що 3) видно дві і тільки дві структури, що входять у жовчний міхур. Іноді анатомічна ідентифікація неможлива, тому ризик ушкодження жовчних шляхів вважається занадто великим. Критичний погляд на безпеку може бути досягнутий у більшості випадків під час лапароскопічної холецистектомії. Однак його погане розуміння та низький рівень сприйняття серед практикуючих хірургів є глобальними проблемами. Підвищення обізнаності щодо критичного погляду на безпеку може збільшити його використання у рутинній хірургічній практиці.
Laparoscopic cholecystectomy is associated with a higher incidence of biliary/vasculary injuries than open cholecystectomy. Anatomical misperception is the most common underlying mechanism of such injuries. The critical view of safety (CVS) has been shown to be a good way of getting secure anatomical identification. It is highly recommended by various guidelines. Conceptually, CVS is a method of target identification, with the targets being the two cystic structures. It entails three basic steps as follows: 1) complete clearance of fibrous and fatty tissue from the hepatocystic triangle, 2) separation of the lower part of the gallbladder from the cystic plate, so that 3) two and only two structures are seen entering the gallbladder. Sometimes, anatomic identification is not possible because the risk of biliary injury is judged to be too great. The critical view of safety can be achieved in most cases during laparoscopic cholecystectomy. However, its poor understanding and low adoption rates among practicing surgeons have been global problems. Increasing awareness about the critical view of safety can increase its use in routine surgical practice.
лапароскопічна холецистектомія; печінково-міхуровий трикутник; міхурова протока; міхурова артерія; міхурова пластинка; критичний погляд на безпеку
laparoscopic cholecystectomy; hepatocystic triangle; cystic duct; cystic artery; cystic plate; critical view of safety
Для ознакомления с полным содержанием статьи необходимо оформить подписку на журнал.
- Purzner RH, Ho KB, Al-Sukhni E, Jayaraman S. Safe laparoscopic subtotal cholecystectomy in the face of severe inflammation in the cystohepatic triangle: a retrospective review and proposed management strategy for the difficult gallbladder. Can J Surg. 2019 Dec 1;62(6):402-411. doi: 10.1503/cjs.014617.
- Fischer L, Kolb G, Segendorf C, Huber B, Watrinet K, Horoba L, Huck B, Schultze D et al. [Which patient needs controls of laboratory values after elective laparoscopic cholecystectomy? — Can a score help?]. Chirurg. 2021 Apr;92(4):369-373. doi: 10.1007/s00104-020-01258-9.
- Fischer L, Watrinet K, Kolb G, Segendorf C, Huber B, Huck B. [After inconspicuous elective laparoscopic cholecystectomy patients can be discharged without control of laboratory parameters]. Chirurgie (Heidelb). 2022 Nov;93(11):1089-1094. doi: 10.1007/s00104-022-01713-9.
- Taki-Eldin A, Badawy AE. Outcome оf Laparoscopic Cholecystectomy іn Patients with Gallstone Disease аt а Secondary Level Care Hospital. Arq Bras Cir Dig. 2018 Jun 21;31(1):e1347. doi: 10.1590/0102-672020180001e1347.
- Kimura Y, Takada T, Strasberg SM, Pitt HA, Gouma DJ, Garden OJ, et al. TG13 current terminology, etiology, and epidemiology of acute cholangitis and cholecystitis. J Hepatobiliary Pancreat Sci. 2013 Jan;20(1):8-23. doi: 10.1007/s00534-012-0564-0.
- Pesce A, Palmucci S, La Greca G, Puleo S. Iatrogenic bile duct injury: impact and management challenges. Clin Exp Gastroenterol. 2019 Mar 6;12:121-128. doi: 10.2147/CEG.S169492.
- Brunt LM, Deziel DJ, Telem DA, Strasberg SM, Aggarwal R, Asbun H, et al. Safe Cholecystectomy Multi-society Practice Guideline and State of the Art Consensus Conference on Prevention of Bile Duct Injury During Cholecystectomy. Ann Surg. 2020 Jul;272(1):3-23. doi: 10.1097/SLA.0000000000003791.
- deʼAngelis N, Catena F, Memeo R, Coccolini F, Martínez-Pérez A, Romeo OM, et al. 2020 WSES guidelines for the detection and management of bile duct injury during cholecystectomy. World J Emerg Surg. 2021 Jun 10;16(1):30. doi: 10.1186/s13017-021-00369-w.
- Nassar AHM, Ng HJ, Wysocki AP, Khan KS, Gil IC. Achieving the critical view of safety in the difficult laparoscopic cholecystectomy: a prospective study of predictors of failure. Surg Endosc. 2021 Nov;35(11):6039-6047. doi: 10.1007/s00464-020-08093-3.
- Mayumi T, Okamoto K, Takada T, Strasberg SM, Solomkin JS, Schlossberg D, et al. Tokyo Guidelines 2018: management bundles for acute cholangitis and cholecystitis. J Hepatobiliary Pancreat Sci. 2018 Jan;25(1):96-100. doi: 10.1002/jhbp.519.
- Strasberg SM. A three-step conceptual roadmap for avoiding bile duct injury in laparoscopic cholecystectomy: an invited perspective review. J Hepatobiliary Pancreat Sci. 2019 Apr;26(4):123-127. doi: 10.1002/jhbp.616.
- Kurahashi S, Komatsu S, Matsumura T, Fukami Y, Arikawa T, Saito T, et al. A novel classification of aberrant right hepatic ducts ensures a critical view of safety in laparoscopic cholecystectomy. Surg Endosc. 2020 Jul;34(7):2904-2910. doi: 10.1007/s00464-020-07610-8.
- Silva Filho JFRE, Coelho GR, Leite Filho JAD, Costa PEG, Barros MAP, Garcia JHP. Liver Transplantation for Bile Duct Injury аfter Cholecystectomy. Arq Gastroenterol. 2019 Sep 30;56(3):300-303. doi: 10.1590/S0004-2803.201900000-56.
- Doğan C, Borazan E, Yılmaz L, Balık AA. How much is the long-term quality of life impaired in cholecystectomy-related biliary tract injury? Turk J Surg. 2023 Mar 3;39(1):34-42. doi: 10.47717/turkjsurg.2023.5780.
- Mosconi C, Calandri M, Mirarchi M, Vara G, Breatta AD, Cappelli A, et al. Percutaneous management of postoperative Bile leak after hepato-pancreato-biliary surgery: A multi-center experience. HPB (Oxford). 2021 Oct;23(10):1518-1524. doi: 10.1016/j.hpb.2021.02.014.
- van Dijk AH, Donkervoort SC, Lameris W, de Vries E, Eijsbouts QAJ, Vrouenraets BC, et al. Short- and Long-Term Outcomes after a Reconstituting and Fenestrating Subtotal Cholecystectomy. J Am Coll Surg. 2017 Sep;225(3):371-379. doi: 10.1016/j.jamcollsurg.2017.05.016.
- Alius C, Serban D, Bratu DG, Tribus LC, Vancea G, Stoica PL, et al. When Critical View of Safety Fails: A Practical Perspective on Difficult Laparoscopic Cholecystectomy. Medicina (Kaunas). 2023 Aug 19;59(8):1491. doi: 10.3390/medicina59081491.
- Nassar AHM, Hodson J, Ng HJ, Vohra RS, Katbeh T, Zino S, et al. Predicting the difficult laparoscopic cholecystectomy: development and validation of a pre-operative risk score using an objective operative difficulty grading system. Surg Endosc. 2020 Oct;34(10):4549-4561. doi: 10.1007/s00464-019-07244-5.
- Griffiths EA, Hodson J, Vohra RS, Marriott P; CholeS Study Group; Katbeh T, et al. Utilisation of an operative difficulty grading scale for laparoscopic cholecystectomy. Surg Endosc. 2019 Jan;33(1):110-121. doi: 10.1007/s00464-018-6281-2.
- Madni TD, Leshikar DE, Minshall CT, Nakonezny PA, Cornelius CC, Imran JB, et al. The Parkland grading scale for cholecystitis. Am J Surg. 2018 Apr;215(4):625-630. doi: 10.1016/j.amjsurg.2017.05.017.
- Sugrue M, Coccolini F, Bucholc M, Johnston A; Contributors from WSES. Intra-operative gallbladder scoring predicts conversion of laparoscopic to open cholecystectomy: A WSES prospective collaborative study. World J Emerg Surg. 2019 Mar 14;14:12. doi: 10.1186/s13017-019-0230-9.
- Sugrue M, Sahebally SM, Ansaloni L, Zielinski MD. Grading operative findings at laparoscopic cholecystectomy- a new scoring system. World J Emerg Surg. 2015 Mar 8;10:14. doi: 10.1186/s13017-015-0005-x.
- Wakabayashi G., Iwashita Y., Hibi T., Takada T., Strasberg S.M., Asbun H.J., et al. Tokyo Guidelines 2018: Surgical management of acute cholecystitis: Safe steps in laparoscopic cholecystectomy for acute cholecystitis (with videos). J Hepatobiliary Pancreat Sci. 2018 Jan;25(1):73-86. doi: 10.1002/jhbp.517.
- Gupta V. Vanishing Calot Syndrome: Common Face of Many Problems. J Am Coll Surg. 2020 Jul;231(1):187-188. doi: 10.1016/j.jamcollsurg.2020.04.002.
- Gupta V. How to achieve the critical view of safety for safe laparoscopic cholecystectomy: Technical aspects. Ann Hepatobiliary Pancreat Surg. 2023 May 31;27(2):201-210. doi: 10.14701/ahbps.22-064.
- Gupta V, Jain G. Safe laparoscopic cholecystectomy: Adoption of universal culture of safety in cholecystectomy. World J Gastrointest Surg. 2019 Feb 27;11(2):62-84. doi: 10.4240/wjgs.v11.i2.62.
- Strasberg SM, Hertl M, Soper NJ. An analysis of the problem of biliary injury during laparoscopic cholecystectomy. J Am Coll Surg. 1995 Jan;180(1):101-25. PMID: 8000648.
- Gupta V, Lal P, Vindal A, Singh R, Kapoor VK. Knowledge of the Culture of Safety in Cholecystectomy (COSIC) Among Surgical Residents: Do We Train Them Well For Future Practice? World J Surg. 2021 Apr;45(4):971-980. doi: 10.1007/s00268-020-05911-6.
- Fischer L, Halavach K, Huck B, Kolb G, Huber B, Segen-dorf C, et al. [The clinical importance of the critical view of safety in laparoscopic cholecystectomy]. Chirurgie (Heidelb). 2023 Jun;94(6):544-549. doi: 10.1007/s00104-023-01833-w.
- Nichols C, Dilday J, Martin M. Tips and Tricks to Avoiding Iatrogenic Bile Duct Injuries during Cholecystectomy. Panam J Trauma Crit Care Emerg Surg 2022;11(3):123-133. doi: 10.5005/jp-journals-10030-1406.
- Majumder A, Altieri MS, Brunt LM. How do I do it: laparoscopic cholecystectomy. Ann Laparosc Endosc Surg. 2020;5:15. doi: 10.21037/ales.2020.02.06.
- Ibrarullah M, Mohanty L, Mishra A, Panda A, Sikora SS. Anatomical appraisal of safe cholecystectomy: a prospective study. ANZ J Surg. 2023 May;93(5):1329-1334. doi: 10.1111/ans.18387.
- Andall RG, Matusz P, du Plessis M, Ward R, Tubbs RS, Loukas M. The clinical anatomy of cystic artery variations: a review of over 9800 cases. Surg Radiol Anat. 2016 Jul;38(5):529-39. doi: 10.1007/s00276-015-1600-y.
- Mischinger HJ., Wagner D., Kornprat P., Bacher H, Werkgartner G. The “critical view of safety (CVS)” cannot be applied — What to do? Strategies to avoid bile duct injuries. Eur Surg. 2021:53:99-105. doi: 10.1007/s10353-020-00660-1.
- Gündüz N, Doğan MB, Alacagöz M, Yağbasan M, Söylemez UPO, Atalay B. Anatomical variations of cystic duct insertion and their relationship with choledocholithiasis: An MRCP study. Egypt J Radiol Nucl Med. 2021;52:202. doi: 10.1186/s43055-021-00579-x.
- Santos BF, Brunt LM, Pucci MJ.The Difficult Gallbladder: A Safe Approach to a Dangerous Problem. J Laparoendosc Adv Surg Tech A. 2017 Jun;27(6):571-578. doi: 10.1089/lap.2017.0038.
- Shang P, Liu B, Li X, Miao J, Lv R, Guo W. A practical new strategy to prevent bile duct injury during laparoscopic cholecystectomy. A single-center experience with 5539 cases. Acta Cir Bras. 2020;35(6):e202000607. doi: 10.1590/s0102-865020200060000007.
- Strasberg SM, Brunt LM. Rationale and use of the critical view of safety in laparoscopic cholecystectomy. J Am Coll Surg. 2010 Jul;211(1):132-8. doi: 10.1016/j.jamcollsurg.2010.02.053.
- The Sages Safe Cholecystectomy Program Strategies for Minimizing Bile Duct Injuries: Adopting a Universal Culture of Safety in Cholecystectomy [(accessed on 1 July 2023)]. Available online: https://www.sages.org/safe-cholecystectomy-program.
- Deng SX, Zhu A, Tsang M, Greene B, Jayaraman S. Sta-ying safe with laparoscopic cholecystectomy: The use of landmarking and intraoperative time-outs. Art Surg. 2021;5:1. doi: 10.21037/aos-21-1.
- Gadiyaram S, Nachiappan M. Fat clearance in the hepatocystic triangle during laparoscopic cholecystectomy: Fact or fad? An NIRF-based study. Asian J Endosc Surg. 2023 Jul;16(3):368-375. doi: 10.1111/ases.13165.
- Honda G, Hasegawa H, Umezawa A. Universal safe procedure of laparoscopic cholecystectomy standardized by exposing the inner layer of the subserosal layer (with video). J Hepatobiliary Pancreat Sci. 2016 Sep;23(9):E14-9. doi: 10.1002/jhbp.382.
- Deziel DJ, Veenstra BR. Biliary Anatomy. In: HJ Asbun, MM Shah, EP Ceppa, ED Auyang, eds. The SAGES Manual of Biliary Surgery. Springer International Publishing, 2020:5-23. doi: 10.1007/978-3-030-13276-7_2.