Журнал «Здоровье ребенка» Том 19, №2, 2024
Вернуться к номеру
Метаболічно асоційована жирова хвороба/метаболічно асоційована стеатотична хвороба печінки: загальні положення
Авторы: Абатуров О.Є., Нікуліна А.О.
Дніпровський державний медичний університет, м. Дніпро, Україна
Рубрики: Педиатрия/Неонатология
Разделы: Справочник специалиста
Версия для печати
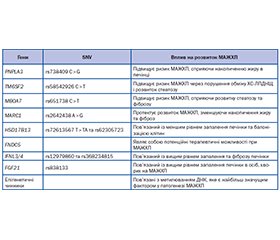
Літературний огляд присвячений недостатньо вивченій у дитячій гастроентерології проблемі метаболічно асоційованої жирової хвороби печінки. До недавнього часу первинний стеатоз печінки, що не асоційований з прийомом алкоголю, визначався як неалкогольна жирова хвороба печінки. З огляду на єдність патогенетичних механізмів, які лежать в основі розвитку первинного стеатозу, пов’язаних з ним стеатогепатиту, фіброзу печінки з метаболічними порушеннями, як-от вісцеральне ожиріння, інсулінорезистентність, метазапалення жирової тканини, було запропоновано змінити термінологію. Авторами наведені дані стосовно сучасних номенклатурних дефініцій, етіологічних факторів, поширеності, критеріїв метаболічних порушень та метазапалення, асоційованих з цією нозологією та характерних саме для дитячого віку. Метаболічно асоційована жирова хвороба печінки та неалкогольна жирова хвороба печінки характеризуються розвитком гепатостеатозу. Відмінною ознакою метаболічно асоційованої жирової хвороби є наявність метаболічних порушень у хворого. Вважають, що використання в клінічній практиці терміна «метаболічно асоційована жирова хвороба печінки» дозволяє лікарям вірогідніше встановлювати діагноз і точніше модифікувати спосіб життя хворого. Велика увага приділена опису гетерогенності метаболічно асоційованої жирової хвороби печінки в клінічній практиці та наведено стислий перелік терапевтичних можливостей щодо метаболічно асоційованої жирової хвороби печінки в дитячому віці.
The literature review deals with the problem of metabolic dysfunction-associated fatty liver disease that is poorly studied in pediatric gastroenterology. Until recently, primary hepatic steatosis not associated with alcohol intake was defined as non-alcoholic fatty liver disease. Given the unity of the pathogenetic mechanisms underlying primary steatosis, associated steatohepatitis, liver fibrosis with metabolic disorders, such as visceral obesity, insulin resistance, meta-inflammation of adipose tissue, it was proposed to change the terminology. The authors present data on modern nomenclature definitions, etiological factors, prevalence, criteria of metabolic disorders and meta-inflammation associated with this nosology and specific to childhood. Metabolic dysfunction-associated fatty liver disease and nonalcoholic fatty liver disease are characterized by the development of hepatosteatosis. However, a distinguishing feature of metabolic dysfunction-associated fatty liver disease is the presence of metabolic disorders in a patient. It is believed that the use of the term “metabolic dysfunction-associated fatty liver disease” in clinical practice allows doctors to make a diagnosis more reliably and more accurately modify the patient’s lifestyle. Much attention is paid to the description of the heterogeneity of metabolic dysfunction-associated fatty liver disease in clinical practice, and a concise list of therapeutic options for metabolic dysfunction-associated fatty liver disease in childhood is presented.
метаболічно асоційована жирова хвороба печінки; неалкогольна жирова хвороба печінки; метаболічно асоційована стеатотична хвороба печінки; ожиріння; діти; огляд
metabolic dysfunction-associated fatty liver disease; non-alcoholic fatty liver disease; metabolic dysfunction-associated steatotic liver disease; obesity; children; review
Для ознакомления с полным содержанием статьи необходимо оформить подписку на журнал.
- Gutiérrez-Cuevas J., Santos A., Armendariz-Borunda J. Pathophysiological Molecular Mechanisms of Obesity: A Link between MAFLD and NASH with Cardiovascular Diseases. Int. J. Mol. Sci. 2021 Oct 27. 22(21). 11629. doi: 10.3390/ijms222111629.
- Ludwig J., Viggiano T.R., McGill D.B., Oh B.J. Nonalcoholic steatohepatitis: Mayo Clinic experiences with a hitherto unnamed disease. Mayo Clin. Proc. 1980 Jul. 55(7). 434-8. PMID: 7382552.
- Lindenmeyer C.C., McCullough A.J. The Natural History of Nonalcoholic Fatty Liver Disease-An Evolving View. Clin. Liver Dis. 2018 Feb. 22(1). 11-21. doi: 10.1016/j.cld.2017.08.003.
- Lonardo A., Leoni S., Alswat K.A., Fouad Y. History of Nonalcoholic Fatty Liver Disease. Int. J. Mol. Sci. 2020 Aug 16. 21(16). 5888. doi: 10.3390/ijms21165888.
- Eslam M., Sanyal A.J., George J.; International Consensus Panel. MAFLD: A Consensus-Driven Proposed Nomenclature for Metabolic Associated Fatty Liver Disease. Gastroenterology. 2020 May. 158(7). 1999-2014.e1. doi: 10.1053/j.gastro.2019.11.312.
- Attia D., Aty N.A., Shawket A., Said E., Fouad Y. MAFLD Not NAFLD is Associated with Impairment of Health-related Quality of Life. J. Clin. Transl. Hepatol. 2022 Feb 28. 10(1). 4-5. doi: 10.14218/JCTH.2021.00485.
- Devarbhavi H., Asrani S.K., Arab J.P., Nartey Y.A., Pose E., Kamath P.S. Global burden of liver disease: 2023 update. J. Hepatol. 2023 Aug. 79(2). 516-537. doi: 10.1016/j.jhep.2023.03.017.
- Sangro P., de la Torre Aláez M., Sangro B., D’Avola D. Metabolic dysfunction-associated fatty liver disease (MAFLD): an update of the recent advances in pharmacological treatment. J. Physiol. Biochem. 2023. 79(4). 869-879. doi: 10.1007/s13105-023-00954-4.
- Gofton C., Upendran Y., Zheng M.H., George J. MAFLD: How is it different from NAFLD? Clin. Mol. Hepatol. 2023 Feb. 29(Suppl). S17-S31. doi: 10.3350/cmh.2022.0367.
- Machado M.V., Cortez-Pinto H. NAFLD, MAFLD and obesity: brothers in arms? Nat. Rev. Gastroenterol. Hepatol. 2023 Feb. 20(2). 67-68. doi: 10.1038/s41575-022-00717-4.
- Méndez-Sánchez N., Bugianesi E., Gish R.G., Lammert F., Tilg H., Nguyen M.H., Sarin S.K., et al.; Global multi-stakeholder consensus on the redefinition of fatty liver disease. Global multi-stakeholder endorsement of the MAFLD definition. Lancet Gastroenterol. Hepatol. 2022 May. 7(5). 388-390. doi: 10.1016/S2468-1253(22)00062-0.
- Eslam M., Newsome P.N., Sarin S.K., Anstee Q.M., Targher G., Romero-Gomez M., Zelber-Sagi S., et al. A new definition for metabolic dysfunction-associated fatty liver disease: An international expert consensus statement. J. Hepatol. 2020 Jul. 73(1). 202-209. doi: 10.1016/j.jhep.2020.03.039.
- Younossi Z.M., Alqahtani S.A., Alswat K., Yilmaz Y., Keklikkiran C., Funuyet-Salas J., et al. Global survey of stigma among physicians and patients with nonalcoholic fatty liver disease. J. Hepatol. 2024 Mar. 80(3). 419-430. doi: 10.1016/j.jhep.2023.11.004.
- Абатуров О.Є., Нікуліна А.О. Метаболічно асоційована жирова хвороба печінки у дітей. Дніпро: ЛІРА, 2021. 724 с.
- Chakravarthy M.V., Neuschwander-Tetri B.A. The metabolic basis of nonalcoholic steatohepatitis. Endocrinol. Diabetes Metab. 2020. 3(4). e00112. Published 2020 Feb 24. doi: 10.1002/edm2.112.
- Byrne C.D., Targher G. MASLD, MAFLD, or NAFLD criteria: have we re-created the confusion and acrimony surrounding metabolic syndrome? Metab. Target Organ Damage. 2024. 4. 10. doi.org/10.20517/mtod.2024.06.
- Rinella M.E., Lazarus J.V., Ratziu V., Francque S.M., Sanyal A.J., Kanwal F., Romero D., et al. NAFLD Nomenclature consensus group. A multisociety Delphi consensus statement on new fatty liver disease nomenclature. Hepatology. 2023 Dec 1. 78(6). 1966-1986. doi: 10.1097/HEP.0000000000000520.
- Vargas M., Cardoso Toniasso S.C., Riedel P.G., Baldin C.P., Dos Reis F.L., Pereira R.M., et al. Metabolic disease and the liver: A review. World J. Hepatol. 2024 Jan 27. 16(1). 33-40. doi: 10.4254/wjh.v16.i1.33.
- Chan W.K., George J. Metabolic fatty liver syndromes: where do we stand in 2024? J. Gastroenterol. Hepatol. Published online February 15, 2024. doi: 10.1111/jgh.16507.
- Alabdul Razzak I., Noureddin M., Trivedi H.D. From Nonalcoholic Fatty Liver Disease to Metabolic Dysfunction-Associated Steatotic Liver Disease: Out with the Old, in with the New. Journal of Clinical Medicine. 2024. 13(3). 880. doi.org/10.3390/jcm13030880.
- Xian Y.X., Weng J.P., Xu F. MAFLD vs. NAFLD: shared features and potential changes in epidemiology, pathophysiology, diagnosis, and pharmacotherapy. Chin Med. J. (Engl). 2020 Dec 14. 134(1). 8-19. doi: 10.1097/CM9.0000000000001263.
- Kim D., Perumpail B.J., Alshuwaykh O., Dennis B.B., Cholankeril G., Ahmed A. Changing trends in aetiology-based hospitalizations with end-stage liver disease in the United States from 2016 to 2019. Liver Int. 2022. 42(11). 2390-2395. doi: 10.1111/liv.15381.
- Habibullah M., Jemmieh K., Ouda A., Haider M.Z., Malki M.I., Elzouki A.N. Metabolic-associated fatty liver disease: a selective review of pathogenesis, diagnostic approaches, and therapeutic strategies. Front. Med. (Lausanne). 2024 Jan 23. 11. 1291501. doi: 10.3389/fmed.2024.1291501.
- Riazi K., Azhari H., Charette J.H., Underwood F.E., King J.A., Afshar E.E., Swain M.G., et al. The prevalence and incidence of NAFLD worldwide: a systematic review and meta-analysis. Lancet Gastroenterol. Hepatol. 2022 Sep. 7(9). 851-861. doi: 10.1016/S2468-1253(22)00165-0.
- Lazarus J.V., Mark H.E., Allen A.M., Arab J.P., Carrieri P., Noureddin M., Alazawi W., et al; Healthy Livers, Healthy Lives Collaborators. A global research priority agenda to advance public health responses to fatty liver disease. J. Hepatol. 2023 Sep. 79(3). 618-634. doi: 10.1016/j.jhep.2023.04.035.
- Murag S., Ahmed A., Kim D. Recent Epidemiology of Nonalcoholic Fatty Liver Disease. Gut Liver. 2021. 15(2). 206-216. doi: 10.5009/gnl20127.
- Lonardo A., Byrne C.D., Caldwell S.H., Cortez-Pinto H., Targher G. Global epidemiology of nonalcoholic fatty liver disease: Meta-analytic assessment of prevalence, incidence, and outcomes. Hepatology. 2016. 64(4). 1388-1389. doi: 10.1002/hep.28584.
- Rinella M., Charlton M. The globalization of nonalcoholic fatty liver disease: Prevalence and impact on world health. Hepatology. 2016. 64(1). 19-22. doi: 10.1002/hep.28524.
- Chen Y.Y., Yeh M.M. Non-alcoholic fatty liver disease: A review with clinical and pathological correlation. J. Formos Med. Assoc. 2021. 120(1 Pt 1). 68-77. doi: 10.1016/j.jfma.2020.07.006.
- Estes C., Razavi H., Loomba R., Younossi Z., Sanyal A.J. Modeling the epidemic of nonalcoholic fatty liver disease demonstrates an exponential increase in burden of disease. Hepatology. 2018. 67(1). 123-133. doi: 10.1002/hep.29466.
- Younossi Z., Anstee Q.M., Marietti M., Hardy T., Henry L., Eslam M., George J., et al. Global burden of NAFLD and NASH: trends, predictions, risk factors and prevention. Nat. Rev. Gastroenterol. Hepatol. 2018 Jan. 15(1). 11-20. doi: 10.1038/nrgastro.2017.109.
- Perumpail B.J., Khan M.A., Yoo E.R., Cholankeril G., Kim D., Ahmed A. Clinical epidemiology and disease burden of nonalcoholic fatty liver disease. World J. Gastroenterol. 2017. 23(47). 8263-8276. doi: 10.3748/wjg.v23.i47.8263.
- Gruneau L., Kechagias S., Sandström P., Ekstedt M., Henriksson M. Cost-effectiveness analysis of noninvasive tests to identify advanced fibrosis in non-alcoholic fatty liver disease. Hepatol Commun. 2023 Jun 22. 7(7). e00191. doi: 10.1097/HC9.0000000000000191.
- Allen A.M., Van Houten H.K., Sangaralingham L.R., Talwalkar J.A., McCoy R.G. Healthcare Cost and Utilization in Nonalcoholic Fatty Liver Disease: Real-World Data From a Large U.S. Claims Database. Hepatology. 2018 Dec. 68(6). 2230-2238. doi: 10.1002/hep.30094.
- Cusi K., Isaacs S., Barb D., Basu R., Caprio S., Garvey W.T., Kashyap S., et al. American Association of Clinical Endocrinology Clinical Practice Guideline for the Diagnosis and Management of Nonalcoholic Fatty Liver Disease in Primary Care and Endocrinology Clinical Settings: Co-Sponsored by the American Association for the Study of Liver Diseases (AASLD). Endocr. Pract. 2022 May. 28(5). 528-562. doi: 10.1016/j.eprac.2022.03.010.
- Yu E.L., Golshan S., Harlow K.E., Angeles J.E., Durelle J., Goyal N.P., Newton K.P., et al. Prevalence of Nonalcoholic Fatty Liver Disease in Children with Obesity. J. Pediatr. 2019 Apr. 207. 64-70. doi: 10.1016/j.jpeds.2018.11.021.
- Yu E.L., Schwimmer J.B. Epidemiology of Pediatric Nonalcoholic Fatty Liver Disease. Clin. Liver Dis. (Hoboken). 2021 Apr 13. 17(3). 196-199. doi: 10.1002/cld.1027.
- Parsa A.A., Azama K.A., Vawer M., Ona M.A., Seto T.B. Prevalence Study of MASLD in Adolescent and Young Adult Pacific Islanders and Asians Living in Hawai’i. J. Endocr. Soc. 2024. 8(3). bvad165. doi: 10.1210/jendso/bvad165.
- Doycheva I., Zhang T., Amjad W., Thuluvath P.J. Diabetes and Hepatocellular Carcinoma: Incidence Trends and Impact of Liver Di–sease Etiology. J. Clin. Exp. Hepatol. 2020. 10(4). 296-303. doi: 10.1016/j.jceh.2019.11.0048.
- Vetrano E., Rinaldi L., Mormone A., Giorgione C., Galiero R., Caturano A., Nevola R., et al. Non-alcoholic Fatty Liver Disease (NAFLD), Type 2 Diabetes, and Non-viral Hepatocarcinoma: Pathophysiological Mechanisms and New Therapeutic Strategies. Biomedicines. 2023 Feb 6. 11(2). 468. doi: 10.3390/biomedicines11020468.
- Alqahtani S.A., Paik J.M., Biswas R., Arshad T., Henry L., Younossi Z.M. Poor Awareness of Liver Disease Among Adults With NAFLD in the United States. Hepatol. Commun. 2021. 5(11). 1833-1847. doi: 10.1002/hep4.1765.
- Abaturov A., Nikulina A. Role of genetic modification of the PNPLA3 gene in predicting metabolically unhealthy obesity and associated fatty liver disease in children. Eur. J. Clin. Exp. Med. 2023. 21(1). 5-13. doi: 10.15584/ejcem.2023.1.1.
- Shi F., Zhao M., Zheng S., Zheng L., Wang H. Advances in genetic variation in metabolism-related fatty liver disease. Front. Genet. 2023 Sep 11. 14. 1213916. doi: 10.3389/fgene.2023.1213916.
- Herranz J.M., López-Pascual A., Clavería-Cabello A., Uriarte I., Latasa M.U., Irigaray-Miramon A., Adán-Villaescusa E., et al. Comprehensive analysis of epigenetic and epitranscriptomic genes’ expression in human NAFLD. J. Physiol. Biochem. 2023 Nov. 79(4). 901-924. doi: 10.1007/s13105-023-00976-y.
- Valencia-Rodríguez A., Vera-Barajas A., Chávez-Tapia N.C., Uribe M., Méndez-Sánchez N. Looking into a new era for the approach of metabolic (dysfunction) associated fatty liver disease. Looking into a new era for the approach of metabolic (dysfunction) associated fatty liver disease. Ann. Hepatol. 2020. 19(3). 227-229. doi: 10.1016/j.aohep.2020.04.001.
- Shiha G., Alswat K., Al Khatry M., Sharara A.I., Örmeci N., Waked I., Benazzouz M., et al. Nomenclature and definition of metabolic-associated fatty liver disease: a consensus from the Middle East and north Africa. Lancet Gastroenterol. Hepatol. 2021 Jan. 6(1). 57-64. doi: 10.1016/S2468-1253(20)30213-2.
- Flisiak-Jackiewicz M., Bobrus-Chociej A., Wasilewska N., Lebensztejn D.M. From Nonalcoholic Fatty Liver Disease (NAFLD) to Metabolic Dysfunction-Associated Fatty Liver Disease (MAFLD)-New Terminology in Pediatric Patients as a Step in Good Scientific Direction? J. Clin. Med. 2021. 10(5). 924. doi: 10.3390/jcm10050924/.
- Mantovani A., Lombardi R., Cattazzo F., Zusi C., Cappelli D., Dalbeni A. MAFLD and CKD: An Updated Narrative Review. Int. J. Mol. Sci. 2022 Jun 23. 23(13). 7007. doi: 10.3390/ijms23137007.
- Bobrus-Chociej A., Wasilewska N., Harasim-Symbor E., Flisiak-Jackiewicz M., Wojtkowska M., Chabowski A., Lebensztejn D. Lack of change in serum sCD36 concentration in children with non-alcoholic fatty liver disease — A preliminary study. Adv. Med. Sci. 2021 Mar. 66(1). 35-40. doi: 10.1016/j.advms.2020.11.004.
- Nyberg L.M., Cheetham T.C., Patton H.M., Yang S.J., Chiang K.M., Caparosa S.L., Stern J.A., et al. The Natural History of NAFLD, a Community-Based Study at a Large Health Care Delivery System in the United States. Hepatol. Commun. 2020 Oct 24. 5(1). 83-96. doi: 10.1002/hep4.1625.
- Targher G., Byrne C.D., Tilg H. NAFLD and increased risk of cardiovascular disease: clinical associations, pathophysiological mechanisms and pharmacological implications. Gut. 2020. 69(9). 1691-1705. doi: 10.1136/gutjnl-2020-320622.
- Huang T.D., Behary J., Zekry A. Non-alcoholic fatty liver di–sease: a review of epidemiology, risk factors, diagnosis and management. Intern. Med. J. 2020. 50(9). 1038-1047. doi: 10.1111/imj.14709.
- Kumar A., Singh A.K., Panda P.K., Nischal N., Soneja M. Non-alcoholic fatty liver disease diagnosis, grading and staging; a simplified tool for clinicians. Journal of Advances in Medicine. 2017. 6(1). 15-22. 10.5958/2319-4324.2017.00003.7.
- Chen Y.H., Wu W.K., Wu M.S. Microbiota-Associated Therapy for Non-Alcoholic Steatohepatitis-Induced Liver Cancer: A Review. Int. J. Mol. Sci. 2020. 21(17). 5999. doi: 10.3390/ijms21175999.
- Ding Y., Deng Q., Yang M., Niu H., Wang Z., Xia S. Clinical Classification of Obesity and Implications for Metabolic Dysfunction-Associated Fatty Liver Disease and Treatment. Diabetes Metab. Syndr. Obes. 2023 Oct 25. 16. 3303-3329. doi: 10.2147/DMSO.S431251.
- Kuchay M.S., Martínez-Montoro J.I., Choudhary N.S., Fernández-García J.C., Ramos-Molina B. Non-Alcoholic Fatty Liver Disease in Lean and Non-Obese Individuals: Current and Future Challenges. Biomedicines. 2021 Sep 28. 9(10). 1346. doi: 10.3390/biomedicines9101346.
- Ye Q., Zou B., Yeo Y.H., Li J., Huang D.Q., Wu Y., Yang H., Liu C., et al. Global prevalence, incidence, and outcomes of non-obese or lean non-alcoholic fatty liver disease: a systematic review and meta-analysis. Lancet Gastroenterol. Hepatol. 2020 Aug. 5(8). 739-752. doi: 10.1016/S2468-1253(20)30077-7.
- Zhang C., Lin R., Li Z., Yang S., Bi X., Wang H., Aini A., et al. Immune exhaustion of T cells in alveolar echinococcosis patients and its reversal by blocking checkpoint receptor TIGIT in a murine model. Hepatology. 2020 Apr. 71(4). 1297-315.
- Fracanzani A.L., Petta S., Lombardi R., Pisano G., Russello M., Consonni D., Di Marco V., et al. Liver and Cardiovascular Damage in Patients With Lean Nonalcoholic Fatty Liver Disease, and Association With Visceral Obesity. Clin. Gastroenterol. Hepatol. 2017 Oct. 15(10). 1604-1611.e1. doi: 10.1016/j.cgh.2017.04.045.
- Shah P., Rathi P., Mandot A., Pal A., Ahire D. Study and Comparison of Metabolic Profile of Lean and Obese Subjects with Non Alcoholic Fatty Liver Disease. J. Assoc. Physicians India. 2020 Aug. 68(8). 51-54. PMID: 32738842.
- Goya T., Imoto K., Tashiro S., Aoyagi T., Takahashi M., Kurokawa M., Suzuki H., et al. The Efficacy of Tofogliflozin on Metabolic Dysfunction-Associated Fatty Liver Disease. Gastroenterology Insights. 2022. 13(1). 20-26. doi.org/10.3390/gastroent13010003.
- American Diabetes Association Professional Practice Committee. 6. Glycemic Targets: Standards of Medical Care in Diabetes-2022. Diabetes Care. 2022 Jan 1. 45(Suppl. 1). 83-96. doi: 10.2337/dc22-S006.
- Santaliestra-Pasías A.M., González-Gil E.M., Pala V., Intemann T., Hebestreit A., Russo P., Van Aart C., Rise P., Veidebaum T., Molnar D., Tornaritis M., Eiben G., Moreno L.A.; IDEFICS Consortium. Predictive associations between lifestyle behaviours and dairy consumption: The IDEFICS study. Nutr. Metab. Cardiovasc. Dis. 2020 Mar 9. 30(3). 514-522. doi: 10.1016/j.numecd.2019.10.006.
- Tagi V.M., Samvelyan S., Chiarelli F. An update of the consensus statement on insulin resistance in children 2010. Front. Endocrinol. (Lausanne). 2022. 16(13). 1061524. doi: 10.3389/fendo.2022.1061524.
- Elkins C., Fruh S., Jones L., Bydalek K. Clinical Practice Recommendations for Pediatric Dyslipidemia. J. Pediatr. Health Care. 2019 Jul-Aug. 33(4). 494-504. doi: 10.1016/j.pedhc.2019.02.009.
- Godoy-Matos A.F., Valério C.M., Silva Júnior W.S., de Araujo-Neto J.M., Bertoluci M.C. 2024 UPDATE: the Brazilian Diabetes Society position on the management of metabolic dysfunction-associated steatotic liver disease (MASLD) in people with prediabetes or type 2 diabetes [published correction appears in Diabetol. Metab. Syndr. 2024 Feb 28. 16(1). 54]. Diabetol. Metab. Syndr. 2024. 16(1). 23. doi: 10.1186/s13098-024-01259-2.
- Flynn J.T., Kaelber D.C., Baker-Smith C.M., et al; Subcommittee on Screening and Management of High Blood Pressure in Children. Clinical Practice Guideline for Screening and Management of High Blood Pressure in Children and Adolescents. Pediatrics. 2017. 140(3). e20171904. Pediatrics. 2018 Sep. 142(3). e20181739. doi: 10.1542/peds.2018-1739.
- Ahrens W., Moreno L.A., Mårild S, Molnár D., Siani A., De Henauw S., Böhmann J, et al.; IDEFICS consortium. Metabolic syndrome in young children: definitions and results of the IDEFICS study. Int. J. Obes. (Lond). 2014 Sep. 38 Suppl. 2. S4-14. doi: 10.1038/ijo.2014.130.
- Наказ МОЗ України від 24 вересня 2022 р. № 1732 «Про затвердження Стандартів медичної допомоги «Ожиріння у дітей». Режим доступу: https://moz.gov.ua/article/ministry-mandates/nakaz-moz-ukraini-vid-24092022--1732-pro-zatverdzhennja-standartiv--medichnoi-dopomogi-ozhirinnja-u-ditej. Дата звернення: 7 березня 2024 р.
- Nikulina A. Genetic variants of the glucagon-like receptor-1 in obesity. Eur. J. Clin. Exp. Med. 2023. 21(4). 682-691. doi: 10.15584/ej cem.2023.4.16.
- Filipovic B., Marjanovic-Haljilji M., Mijac D., Lukic S., Kapor S., Kapor S., Starcevic A., et al. Molecular Aspects of MAFLD-New Insights on Pathogenesis and Treatment. Curr. Issues Mol. Biol. 2023 Nov 15. 45(11). 9132-9148. doi: 10.3390/cimb45110573.
- Lubrecht J., van Giesen Guusje H.J., Jańczyk W., Zavhorodnia O., Zavhorodnia N., Socha P., Lev H. et al. Pediatricians’ practices and knowledge of metabolic dysfunction-associated steatotic liver disease: An international survey. Journal of Pediatric Gastroenterology and Nutrition. 2024. 1-10. doi: 10.1002/jpn3.12124.